At the American Rheumatology Association’s annual meeting on Sunday, November 6th, I was honored to co-present at a study group called: Promoting an Interdisciplinary Approach to Supporting Persons with Inflammatory Arthritis at Work. “Inflammatory arthritis” (IA) is an umbrella term that includes rheumatoid, psoriatic, ankylosing spondylitis and rheumatic conditions that have systemic effects far beyond joint pain.
Many people wonder: “Can I work with arthritis?” Unfortunately, arthritis does interfere with work for many people, however there are supports that can help. As an occupational therapist living with rheumatoid arthritis, I’d love to provide some resources for understanding the distinct role of occupational therapy in supporting people with inflammatory arthritis at work.
I have also included resources for understanding the roles of other professionals on the multidisciplinary team, and for finding work accommodations and supports for those who aren’t able to access an occupational therapist or other multidisciplinary team member at this time.
What is occupational therapy (OT)?
According to the American Occupational Therapy Association, “Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability. Occupational therapy is the only profession that helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations).”
To an occupational therapist, an “occupation” doesn’t only mean a formal job, an occupation is *any* meaningful activity that an individual needs or wants to perform. It includes the “jobs” that make up your day, like getting dressed, cooking, caring for pets, managing medical appointments, and yes, formal employment tasks.
In the United States, occupational therapists are licensed health professionals in all 50 states and must have a Masters degree to enter the profession.
For an overview of how OT might help someone with arthritis, I outlined twenty-six ways OTs help people with arthritis in this blog post, and the American Occupational Therapy Association has a great handout outlining common interventions for arthritis here.
How can Occupational Therapists help people with Inflammatory Arthritis with Employment and Work?

While some occupational therapists specialize in hand therapy, I like to say that we are “Life Therapists, not only Hand Therapists!”
Occupational therapists don’t just look at what’s going on inside someone’s body, we also look at the fit between the person, their external environment, and that task that they want or need to do.
We then assess where the clients is struggling (internal factors? external environmental factors? a mix of both) and determine whether the factors at play are solvable / changeable or perpetual / unchangeable. If the problem is solvable, we try a remedial strategy (eg hand strengthening for hand weakness). If the problem is not able to be changed (eg a fixed deformity), we attempt to find ways to workaround it. We collaborate closely with our clients to ensure our treatment goals and interventions are meaningful and relevant to their specific context, goals and values.
When should I refer a person with inflammatory arthritis to an occupational therapist?
The simple answer is: whenever the person with arthritis has difficulty participating in work or functioning in their work environment! It really is that simple.
According to the Occupational Therapy Practice Guidelines for Adults with Arthritis and Rheumatic Disease: “Referrals for occupational therapy services can occur during any phase of the disease process when symptoms are interfering with the client’s occupational performance” (Appendix B2, (which simply means the ability to do necessary daily tasks)
Examples of when a person with arthritis might need occupational therapy to support work performance include:
- Increased Fatigue: difficulty sustaining energy throughout the work day
- Poor Dexterity & Increased Pain: difficulty performing work tasks on a computer
- Psychosocial effects: coworkers may not understand fluctuating symptoms, leading to stress
What do occupational therapists assess in an initial evaluation?

- Evaluation of physical factors & performance skills (mental, sensory, movement, process skills – includes cognition, strength and more)
- Evaluation of the fit between the person and their context & environment (cultural, personal, virtual contexts, & social and physical environment – this may include skilled observation of the person performing work related tasks in their context)
- Semi-structured interview including questions like: “What’s a day in your life like? Where are you having difficulty?” The OT will distinguish between tasks the patient is performing successfully & unsuccessfully, and they will attempt to assess what is impeding performance: fatigue, pain, social barriers, environmental barriers, or other factors.
- A discussion about “Performance Patterns” (habits, roles, routines)
- A discussion about the patient’s goals and values.
Common standardized assessments used in an initial occupational therapy evaluation for people with arthritis include:
- Canadian Occupational Performance Measure (COPM), a standardized patient self-report of function “in all areas of life, including self-care, leisure and productivity.”
- Disability index (DI) of the Health Assessment Questionnaire (HAQ)
- Arthritis Impact Measurement Scales 2 (AIMS)
- Fatigue Severity Scale (FSS)
- Hospital Anxiety and Depression Scale (HADS)
- Arthritis Self-Efficacy Scale
- Disabilities of Arm, Shoulder and Hand (DASH)
- Handgrip dynamometry – JAMAR® Dynamometer
- Manual Muscle Testing
What interventions do occupational therapists use to support people with inflammatory arthritis at work?
Our interventions are typically individually tailored to each client’s unique needs, as a result of their in depth evaluation. If an occupational therapist has five different clients with rheumatoid arthritis on her caseload, for example, the goals and treatment strategies will vary vastly depending on each individual client’s goals, internal factors, environmental supports and task demands.
That said, here are some typical interventions used to help people with inflammatory arthritis maintain employment and work more comfortably:
- Fatigue Interventions: This typically includes education on energy conservation and task simplification. For example, we may come up with a schedule that includes taking a 10 minute break after every 50 minutes of work, to help sustain energy. Fatigue interventions can also include therapeutic activities and exercises designed to decrease stiffness and improve endurance and strength.
- Assistive Technologies: this can include training on assistive and augmentative technologies such as “Speech to Text” and an ergonomic keyboard, mouse, chair, and more.
- Educating patients on their rights to accommodations and supporting patients in self-advocacy. This can be crucial for supporting patients with bringing up the topic of needing work accommodations in the first place.
- Task modifications: Occupational therapists suggest ways to modify work materials to reduce pain & fatigue.
- Coping skills: Coping skills for concurrent stress/anxiety, and social intervention, which may include training on mindfulness.
- Psychosocial intervention: educate coworkers / boss on nature of condition (eg unpredictable flare ups and remissions).
- Pain Management: Education on joint protection, Compression garment, hot & cold and other basic pain relief measures.

In the below video you’ll see some simple examples of task modifications that can make handwriting easier for someone with arthritis.
Additional Resources for Work Accommodations and Supports
Here are just a few resources mentioned during our talk, in addition to some more that you might find helpful:
- AskJan.Org – the Job Accommodation Network (JAN) is the leading source of free, expert, and confidential guidance on job accommodations and disability employment issue
- Understanding Accommodations for Arthritis at Work – helpful article by Arthritis Canada
- Know your Workplace Rights if you have a Disability – helpful article by Arthritis Foundation, USA
- Pain Toolkit – some wonderful free self-management resources for patients in pain
- Mindfulness for stress management and coping: UCLA health free mindfulness
- Mindful Self-Compassion Workbook – I have personally found this helpful in coping not only with work stress but also overall life with rheumatic disease.
- Yoga resources: in the chat some people asked for yoga resources and here are two I really like – Yoga for Arthritis and Yoga with Adriene
- I personally run Rheum to THRIVE, an online patient support and education group (self-management group) that gives patients skills to manage all aspects of life with inflammatory arthritis. There is a monthly fee but I accept sliding scale payments including free admission to those who cannot afford it.
Real patient perspectives on the impact of inflammatory arthritis on work participation: it’s NOT just about joint pain!
I’m sharing these perspectives with permission from the respective patients.
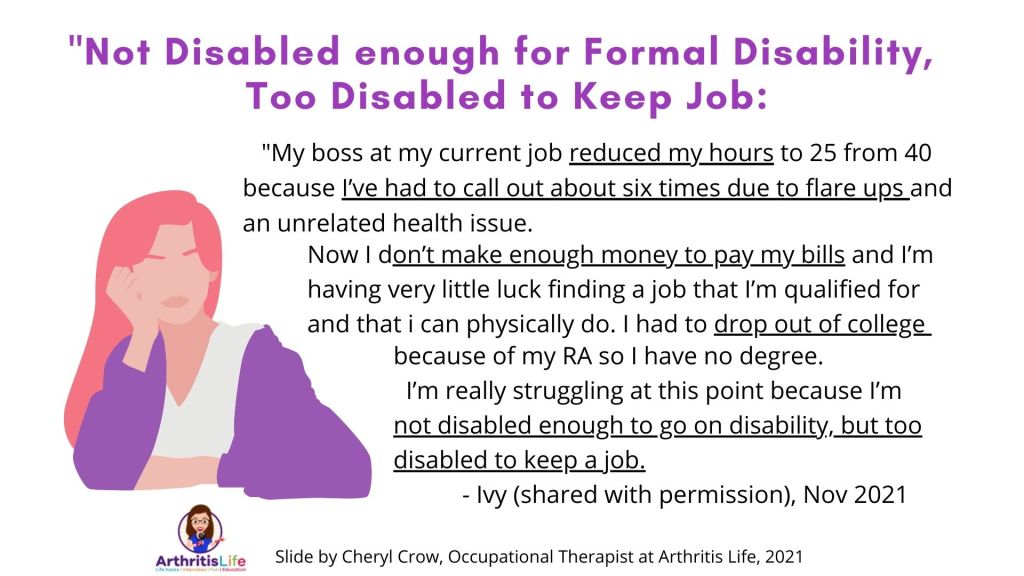
One of the most common themes I’ve observed is the stress of being in the “messy middle” in between fully functional and fully disabled.
“My boss at my current job reduced my hours to 25 from 40 because I’ve had to call out about six times due to flare ups and an unrelated health issue. Now I don’t make enough money to pay my bills and I’m having very little luck finding a job that I’m qualified for and that I can physically do. I had to drop out of college because of my RA so I have no degree.
I’m really struggling at this point because I’m not disabled enough to go on disability, but too disabled to keep a job.” – Ivy (shared with permission), Nov 2021
Two more common challenges are managing unpredictable flare-ups, along with this invisible or unseen nature of inflammatory arthritis and rheumatic disease. These can lead to significant psychosocial challenges with coworkers and loved ones.
“Symptoms are variable, so I may seem completely fine one day but be ill the next. Relatedly, arthritis is an invisible illness. Sometimes, there are concrete indicators like deformed joints or a person wincing in pain, but most of the time a person looks “normal” & forces themselves to function at a “normal” level.
Employers need to stop asking “You couldn’t do that yesterday. why can you do that today?” or even worse questioning a person’s illness.”” – @SimranFrontain, Instagram, Nov 2021
Additionally, deciding whether or not to disclose one’s condition in the workplace can be an extremely confusing and distressing experience, as Claire shares in this interview below (conducted in 2019):
For another example of how arthritis can affect not only one’s work life but one’s deep sense of self and identity, check out minute 25:00 of my interview with James on the Arthritis Life Podcast here.
You can also check out minute 48:00 through the end of my podcast discussion with Joel, where we discussed the difficulty of taking sick leave from work due to rheumatic disease, and how that can lead to feelings of guilt.
Occupational therapists aren’t the only licensed health professionals who can help people with inflammatory arthritis at work!
At this ACR 2021 talk, clinical social workers Joan Westreich and Adena Batterman discussed their role in helping support people with IA at work – check out this article to learn more about clinical social work. Also check out the Early Arthritis Center to see the phenomenal work Joan, Adena and their teammates are doing to support patients.
We also heard from rheumatologist Dr. Vivian Bykerk, who discussed the role of the rheumatologist in proactively addressing work related concerns in rheumatology encounters, and then referring patients to additional supports as needed.
Citations:
- de Almeida PH, Pontes TB, Matheus JP, Muniz LF, da Mota LM. Terapia ocupacional na artrite reumatoide: o que o reumatologista precisa saber? [Occupational therapy in rheumatoid arthritis: what rheumatologists need to know?]. Rev Bras Reumatol. 2015 May-Jun;55(3):272-80. Portuguese. doi: 10.1016/j.rbr.2014.07.008. Epub 2014 Oct 24. PMID: 25440699.
- Macedo, A.M., Oakley, S.P., Panayi, G.S. and Kirkham, B.W. (2009), Functional and work outcomes improve in patients with rheumatoid arthritis who receive targeted, comprehensive occupational therapy. Arthritis & Rheumatism, 61: 1522-1530. https://doi.org/10.1002/art.24563
- Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am J Occup Ther August 2020, Vol. 74(Supplement_2), 7412410010p1–7412410010p87. doi: https://doi.org/10.5014/ajot.2020.74S2001
- Occupational Therapy Practice Guidelines for Adults With Arthritis and Other Rheumatic Conditions (2017), Author(s): Poole, Janet L., PhD, OTR/L, FAOTA; Siegel, Patricia, OTD, OTR/L, CHT; Tencza, Melissa J., MOT, OTR/L, ISBN 13: 978-1-56900-438-8, publisher: AOTA press
- Tang, K., Beaton, D.E., Boonen, A., Gignac, M.A.M. and Bombardier, C. (2011), Measures of work disability and productivity: Rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA), Workplace Activity Limitations Scale (WALS), Work Instability Scale for Rheumatoid Arthritis (RA-WIS), Work Limitations Questionnaire (WLQ), and Work Productivity and Activity Impairment Questionnaire (WPAI). Arthritis Care Res, 63: S337-S349. https://doi.org/10.1002/acr.20633




